Six Important Changes to Expect Under CVS Caremark
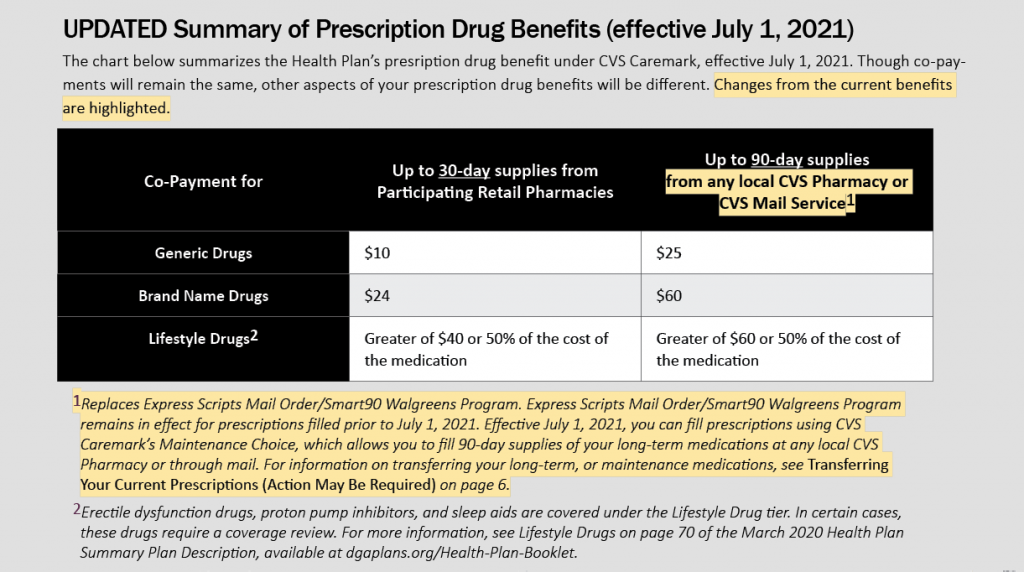
Many aspects of the Health Plan’s prescription drug benefit will remain unchanged following the transition to CVS Caremark. Refer to the chart below, titled Summary of Prescription Drug Benefits, for more details of the changes effective July 1, 2021. Please note there are additional changes that will occur after the July 1st transition, which are discussed in the article titled New Prescription Drug Benefits Available September 1, 2021.
- Pharmacy Network
Choose from more than 68,000 retail pharmacies in the CVS Caremark network to fill your prescriptions and receive the network discount. To locate a network pharmacy in your area, visit Caremark.com, or call CVS Customer Care at (855) 271-6601.
You may also fill prescriptions at a non-network pharmacy. When using a non-network pharmacy, you will not receive the network discount and will need to pay the full cost of the medication. This will also require you to request reimbursement through CVS Caremark.
- Local pickup of 90-day supplies of long-term medications
You can pick up 90-day supplies of long-term medications and pay the mail order co-payment at a local CVS, Longs or Navarro pharmacy location. This option will no longer be available through the Smart90/Walgreens program.
- Mail Order Pharmacy
All mail order prescriptions can be filled by mail through CVS Caremark Mail Service. For information on transferring your current prescriptions, visit Transferring Your Prescriptions (Action May Be Required).
- Appeals Procedure
Your claim will be processed in accordance with the Health Plan’s claims procedures. If your prescription/pre-authorization for a prescription is denied, CVS Caremark will perform the first level appeal and second level appeal. If both appeals are denied by CVS Caremark, you can then submit an appeal to the Health Plan for further consideration. The Health Plan will not consider an appeal unless it has already gone through both levels of appeal with CVS Caremark.
- Specialty Drug Pharmacy
All specialty medications must be filled by CVS Specialty to avoid paying the full drug cost. See page 7 for information on transferring your specialty medications.
- New Prescription Drug Coverage Card(s)
Welcome Kits from CVS Caremark have been mailed to all covered Health Plan participants. This kit will include important information about your prescription drug coverage, including new prescription drug cards for you and your covered dependents.
Be sure to discard your previous coverage card and replace it with the CVS Caremark coverage card when you receive it.
Your new coverage card will include your new prescription drug coverage ID number, which you can then use to register for CVS digital tools. (See Managing Your CVS Caremark Prescriptions With CVS Caremark’s Digital Tools for more information.) Registered users of the CVS Caremark mobile apps can access a digital version of their prescription coverage card on their smartphone as needed.