How To Fill Prescriptions If You Are Covered By Both WGA and DGA Health Plans
Just like your medical benefits, when you have prescription drug coverage with more than one insurer, your prescription drug costs are coordinated between your health plans.
If you have prescription drug coverage with both the Directors Guild of America – Producer Health Plan and the Writer’s Guild of America – Industry Health Fund, your two plans will have different prescription drug managers, effective July 1. Despite this, the Health Plan will continue to coordinate prescription benefits with the WGA Health Fund, to ensure each plan pays its share of costs and you maximize the benefits of both plans to decrease your out-of-pocket responsibility.
Below are step-by-step instructions for submitting your prescriptions so that your prescription drug costs are processed by both plans. The steps below apply to all participants who have prescription drug coverage with more than one insurer.
Prescriptions at CVS Caremark Network Pharmacies
- Determine which plan is considered primary, secondary, tertiary, etc. The Health Plan’s coordination of benefits rules can be found on page 46 of the March 2020 Health Plan Summary Plan Description available at www.dgaplans.org/Health-Plan-Booklet. Note that other plans might have different coordination of benefits rules.
- At the pharmacy, present all applicable prescription drug coverage cards to the pharmacist, informing the pharmacist which is primary, secondary, tertiary, etc.
- The pharmacist should process your prescription in the order based on the coverage hierarchy.
- If the pharmacist has difficulties processing your prescription according to the coordination of benefits hierarchy, have them contact the CVS Pharmacy Help Desk for Pharmacists, using the number on the back of your DGA Health Plan prescription drug coverage card.
Prescriptions at Non-Network Pharmacies
If you fill a prescription at a non-CVS-network pharmacy, you will pay the full cost of the medication and subsequently will need to file a prescription claim for reimbursement of any covered costs. To ensure your claim is processed properly according to the coordination of benefits order, follow the steps below:
- Determine which plan is considered primary, secondary, tertiary, etc. The Health Plan’s coordination of benefits rules can be found on page 46 of the March 2020 Health Plan Summary Plan Description available at www.dgaplans.org/Health-Plan-Booklet. Note that other plans might have different coordination of benefits rules.
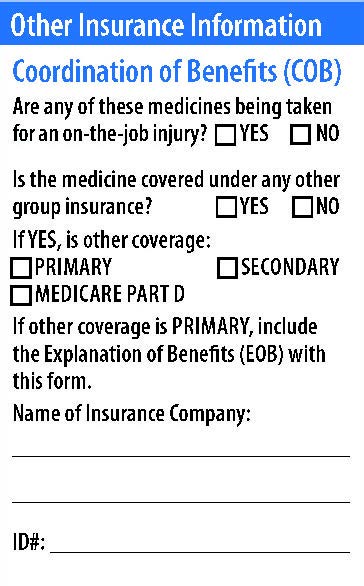
- Complete a CVS Caremark Prescription Reimbursement Claim Form. Provide the appropriate coordination of benefits information in the Other Insurance Information section (pictured below).
- Return your completed prescription claim form to CVS Caremark.
- Please keep in mind that not all health plans offer coordination of benefits or might have different coordination of benefits rules. If you have coverage other than the DGA Health Plan, check with your insurer for more information.