Coordination of Benefits Form Is Required When You Are Covered By the Health Plan
Claims submitted to the Health Plan will be denied if a current Coordination of Benefits form is not on file.
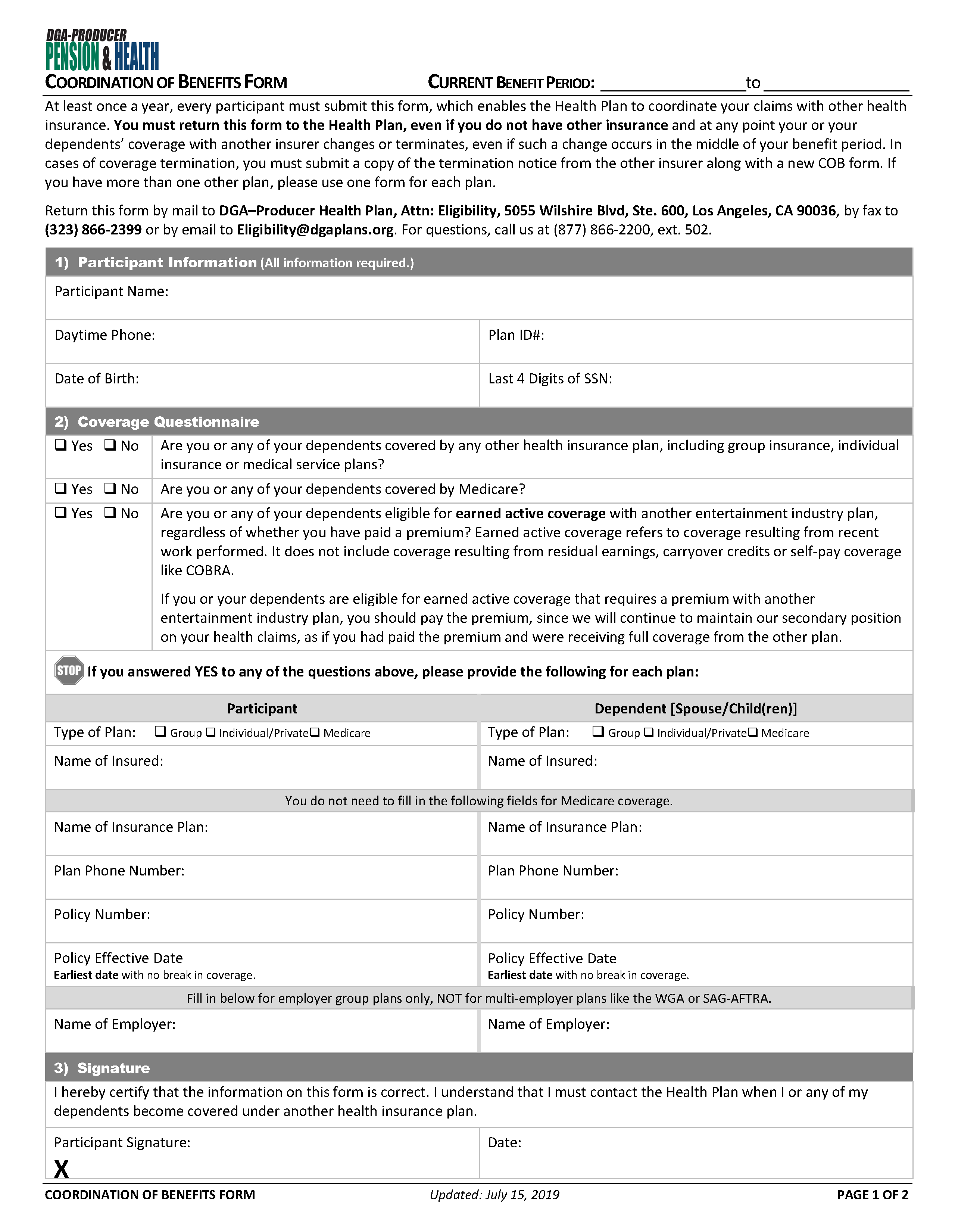
For each year you have Health Plan coverage, you must submit a new Coordination of Benefits (“COB”) form, verifying whether or not you and/or any of your dependents are eligible for coverage from another insurer. This form is included in the open enrollment packet you receive at the beginning of each benefit period and should be completed and returned even if the information has not changed. Without a current COB form on file, your claims and those of your dependents will be denied until a new form is submitted.
Below is a list of frequently asked questions regarding the COB form:
-
Where can I get a COB form?
The COB form is included in your open enrollment package. It is also available on the Plans’ website: www.dgaplans.org under Documents and Forms.
-
Should I include my DGA Health Plan information on the COB form?
No. Only outside insurance information, such as coverage from other entertainment industry health plans, coverage provided by your spouse’s employer, or private plans should be included on the COB form.
-
Should I include Medicare information on the COB form?
You do not need to include Medicare information on the form.
-
Do I need to submit a COB form for each dependent?
No. Only one COB form is required for you and your dependents unless you need additional space to add more information.
-
What happens if I am late submitting my COB form?
If a current COB form is not on file, the Health Plan will deny your claims until a new COB form is submitted.
-
Where can I send the COB form?
A completed COB form can be emailed to eligibility@dgaplans.org, mailed to the address on the form, or faxed to (323) 866-2399.
-
Should I submit a COB form each year, even though there is no change?
Yes. A new COB form is required each year.
-
Can I use a copy of last year’s COB form for the following year if the information is the same?
No. The Health Plan requires a new COB form every year regardless of whether the information on the form has changed.
-
My COB form was received. How long will it take for my denied claim(s) to be reprocessed?
Once the COB form is processed, it takes up to 10 business days for your denied claim(s) to be reprocessed.
-
Do I need a new COB form for each claim denied?
No. Only one COB form for that period is required for each benefit period.